From Tragic Loss to Healing: Soojin Jun Advocates for Better Patient Care by Listening to the Often Unheard
After losing her father to gaps in healthcare, digital artist Soojin Jun went to pharmacy school and became a top voice in patient safety and equity.
I’ve been following
on LinkedIn for some time. In pharmacist circles, Soojin is well-known for her patient safety and advocacy work. She’s also known for her writing, steely activism, and soulful creativity. I’m excited to share Soojin’s voice here.Soojin came to the States from South Korea as a young teen. Her childhood was trauma-filled and became more chaotic after her parents divorced. After moving from the East Coast to the West living with different relatives, Soojin settled in Chicago and was reunited with her father.
In 2002, Soojin earned a digital arts Bachelor's degree from Columbia College Chicago. She began a career as a wedding videographer. Life didn’t settle down for Soojin after marrying and having two kids.
In 2006, she became a ‘sandwich caregiver’ when her father was diagnosed with stage 3 esophageal cancer. An overwhelming experience for anyone, but especially difficult for a young mom with additional barriers: language, cultural, financial, and medical fluency.
Distressed with her father’s poor care, they planned to continue his cancer treatments back in his home country. One week before their trip, her father died of a completely preventable medication side effect — not from his cancer. Soojin saw firsthand how numerous the gaps in healthcare are.
Through this tragic experience, Soojin learned: “I had to start speaking up. Otherwise, there was no one who would speak up for someone like my dad. No one.”
Soojin started on a new path with a new mission: to keep patients and their families safe in every way. She went back to school in her 30s and earned a PharmD from the University of Illinois Chicago.
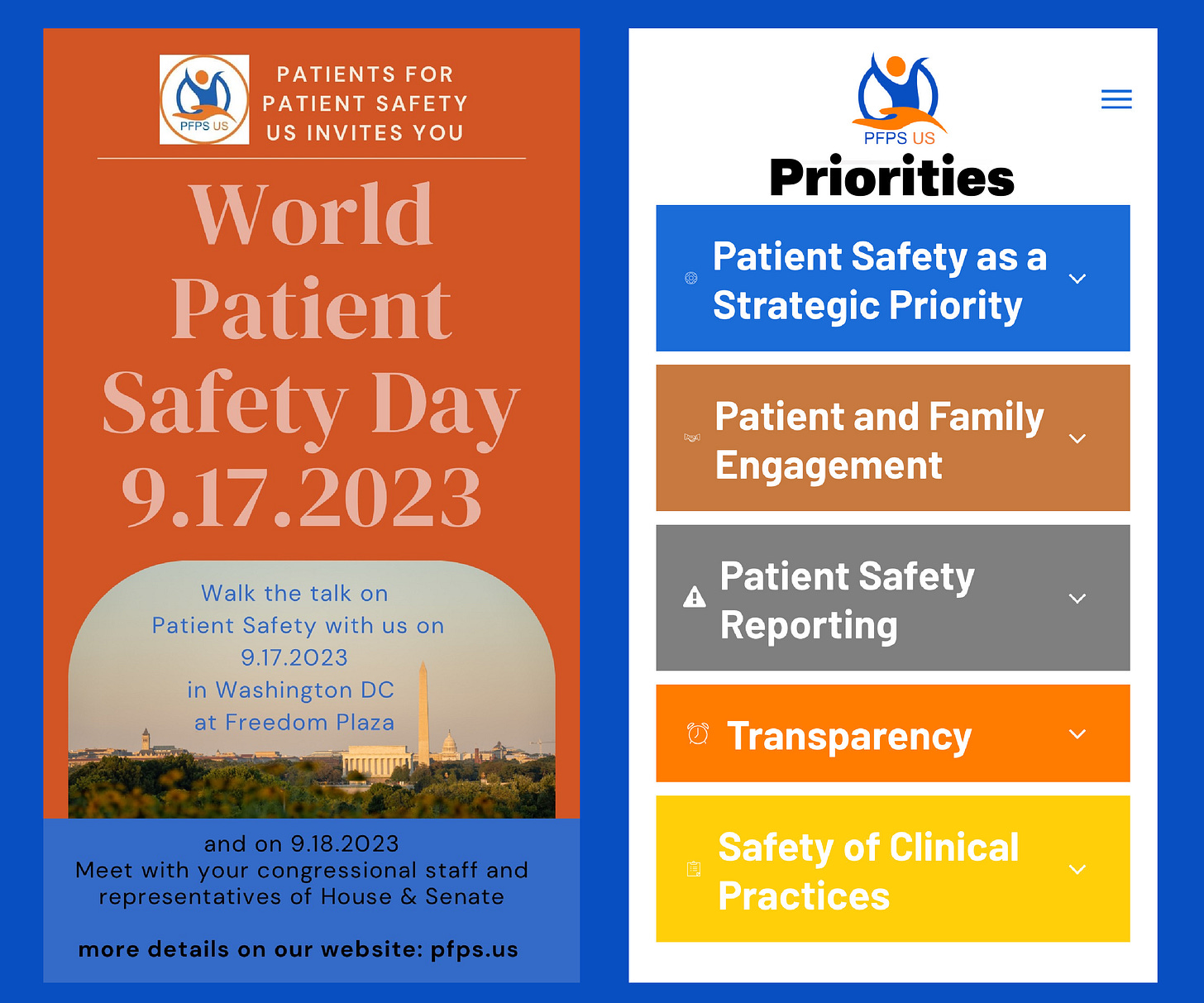
Since then, Soojin has become a top voice in patient safety and equity. She’s cofounder of Patients for Patient Safety US. She’s a Medium writer and publisher of I am Cheese. And in 2022, Soojin was included in Medika Life’s top-30 list of women transforming healthcare.
Working full-time, Soojin specializes in helping older adults manage their medication therapies. She lives in north suburban Chicago with her husband and three children.
Recently, I met up with Soojin in Milwaukee to learn more about her story and mission. She’s even more lovely in person. It was such a delight to hear her perspective on a wide range of topics, including new approaches to thinking about healthcare, facing fear head-on, and healing from trauma.
After spending a decade working in patient safety, what’s the biggest piece of insight you’ve learned and would like to share?
Many people are in a denial loop in the hopes of wanting to believe that healthcare is safe. And this applies from individual level to organizational. That is why I believe starting from self, individual, or one person is crucial before pointing fingers to others. Going deep into the root cause of the issue is something that many people are afraid to do.
In our first conversation, you mentioned that Western medicine is becoming the norm worldwide. And you hinted at some concern about losing the wisdom Eastern medicine has to offer. Can you talk a little bit about that?
Medicine is a soft science if you have to put it in a category of science. To me, it is an art. Art involves creativity and in the case of medicine it also involves emotions, empathy and compassion in the interaction and the process. I often think it is not emphasized enough in Western Medicine, though there are plenty of us who advocate for recognizing the importance of this part.
I understand the concern as many don’t want to “prescribe” methods that are not evidence-based. However, what matters the most is if patients feel healed. And if science-based medicine is not healing patients, then there are other sides…perhaps these are the aspects that Western Medicine keeps denying their existence. I could be biased in a sense since I come from Eastern culture, however.
You describe patient safety as a broad term. How can differences in cultural backgrounds between patients and their providers impact safety?
Differences in cultural backgrounds impact safety deeply for many reasons. We often provide surveys for feedback from patients, for example. For some cultures, however, the concept of survey is unknown to them. I experienced this while conducting a health literacy seminar for a nonprofit.
If there had been empathy and compassion in this interaction, however, we would have done anything and everything to collect feedback. If not, there is no way to collect feedback from these people! And this is how it is currently. In order for health equity to be a reality, we really need to design healthcare with mindfulness.
The remedy, in my humble opinion, is to start from the commonality. We all want to be seen, heard, and understood. So starting from there…how can we make the patient be seen and heard? Just start from there with empathy and compassion…then differences will melt away. We will do anything and everything to come up with solutions.
I believe every patient needs an advocate because of the complexity, cost, and hurdles. The current model of healthcare has no way of understanding what’s going on in patients’ lives.
You advocate for trauma-informed care. Can you describe what it means and explain why it’s needed?
Trauma-informed care will revolutionize how we provide care and will make so many patients feel healed, finally being acknowledged for what they are going through. I personally think all patients need to start from behavioral health counseling to find root causes of what is going on physically.
Trauma-informed care means being aware and acknowledging trauma of the patient, how the trauma can affect the patient and manifest mentally and physically, and providing healing as a whole person with the information in mind rather than just treating the symptoms on the surface.
Many behaviors come from traumas and they may look benign or like some habits to an extent at the surface. However, there are often deeper root causes when patients get sick.

You’ve written about the many gaps in your father’s care. Can you discuss how the lack of clear medical instructions and guidance was a major one?
This is why I believe every patient needs an advocate because of the complexity, cost, and hurdles to jump through. I believe the current model of healthcare has no way of knowing and understanding what is going on in patients’ lives as it is very industrialized. When the task assigned is done, often we don’t think about the patients or have a way of knowing what happened.
My father went to the same hospital for hypoglycemia twice in a row within the span of a month. Shouldn’t that alarm someone at the hospital? No, as there was no mechanism to care in this case, a serious design failure. And he ended up dying two weeks later. Repeated hypoglycemia can be dangerous like his case. Yet, there would be no one who would care to know what happened, except me. If I had no medical knowledge, then I wouldn’t even know there was medical harm.
In a podcast interview with the authors of Love as a Business Strategy, you said, “I guarantee 100% of all patients with language barriers have issues with healthcare.” Why is access to interpreters not enough? And what would better support their communication and safety needs?
The current model supports interpreters in an industrialized way. When you’re done with that interpreter then you may not see that interpreter again. But modern medicine is about dealing with chronic conditions more than acute conditions and this model doesn’t support the chronicity of care needed. When interpreters change with each medical visit, the same information is often repeated!
Also there is no choice within interpreters. Patients with language barriers are expected to accept who is given. What has been said orally in medical communication can be difficult to understand and we don’t necessarily provide information in writing.
And you know how we say things matter. Do all interpreters have proper training in medical communication with empathy and compassion which we demand from staff who speak in English? Can we verify that? Not really.
You’ve been through so many major periods of change. Are you starting to feel more settled or do you feel like change is normal?
Change has been very normal throughout my life and that is probably why I can adapt quite quickly. Being settled is an illusion unless you want to stop growing, which means you are dying then, and that is still a change. Change is inevitable. Life is always ‘-ing’ — in progress.
It’s hard to imagine what that was like for you coming to the States alone and adapting to a new culture during your teen years. Do you look back at that time period differently now?
I feel so many people are seeing their own past experiences through a new lens during the cultural change happening now. It was the most difficult time of my life that I felt so alone and the only hope I could have was God at the time. That faith, although it was very difficult to hold on to, kept me alive and going. I am also grateful to my little brother. I don’t think I would be here without him.
I can’t think of another pharmacist who followed a similar path: art school and then a decade later pharmacy school. How did you manage that, especially with young kids?
Oh, I don’t think I can manage it if I had to do it over!! Three hours of sleep a night was a staple of my life for a very long time. I would not recommend it! Passion for change kept me going and tremendous support from my family. Thanks to the support, I actively participated even in business plan competitions on top of my studies because I couldn’t wait for change to happen.
It was a fun time for me, although it was tiring. In hindsight, I was in the flow of creativity while I was doing that with my friends. I poured all my heart and energy into it and this was more than 10 years ago if you think about it. I was imagining about healthcare that is happening now.
I loved your post explaining how you overcame your fear of rejection as a writer. You say the words given to you by Aussie Medium writer Tim Denning encouraged you to “hit publish and set yourself free.” What has being a part of a community of writers meant to you? And do you still fear rejection?
Community means everything, from your individual being, career, and basically any endeavor you attempt to do. We are social beings and understanding that aspect and owning it will help you in every direction. It doesn’t matter whether you are an introvert or extrovert — often an argument I hear from people who identify themselves as introverted.
See if a trauma response might be finding comfort in the identification process. There are many traumas in our lives that we don’t deal with head-on. Fear of rejection is a natural response and of course I still do have the fear. Taking a mindset that ‘I don’t have to be perfect’ and ‘everything changes in every moment’ will free yourself from being stuck in that fear.
Every first thing involves fear. And even with years of practice of whatever you’re doing, that fear will always be there. It is all about how you show up with readiness because no one can know the reactions of others and the magnitude of how that can affect you.

Community means everything, from your individual being, career, and basically any endeavor you attempt to do.
You’ve talked about how difficult it can be to use words to explain symptoms. Is there anything you’ve found that helps you get in touch with your body?
I have gotten to know Reiki healing a bit more and it is very interesting. Some Reiki practitioners can know the whereabouts of pains and other issues in the body by touching sections of the body or even intuitively and provide a sense of healing.
I know there are many technological solutions being developed in wearable devices, using pictures in progress notes, and I have read a recording from a smartphone that helped a patient for a seizure diagnosis.
You say you’ve become an empath through your patient advocacy work. Do you feel like you absorb other people’s pain and it stays with you?
I am learning skills to create boundaries for myself so I can help more people. I knew it had to start from me. It is the easiest — and the hardest — to work on yourself.
What exactly does cultural sensitivity look like in healthcare interactions? And why is it essential for trust?
There is some confusion around the difference between cultural sensitivity and bias. It is important to look at patients as whole persons who have differences from who we are and honor the differences. Trust can only happen when both sides are open. When one side has bias over cultural sensitivity, then there is an imbalance of openness, and therefore lack of trust.
In 3 Tips on Making Medical Decisions, you write about your lessons learned while caring for your dad. The tip on asking your healthcare provider, “What would you do if you were me?” stood out for me personally. I asked that exact question just as my dermatologist was about to rush out of the exam room, leaving a suspected — and later confirmed — non-melanoma skin cancer on my face.
I put that question out there in a way to force empathy in a healthcare interaction because often clinicians have so much going on…next patient, busy schedule, unresolved cases, etc. The way the workflow is designed for providers is completely chaotic. Or is it even designed? Saying “What would you do if you were me?” is a way patients can demand “Look at me, hear me, think of me.” It’s not perfect but I would still recommend it.
You’ve made some pretty big career shifts. Going from a wedding videographer in your 20s to a pharmacist in your 30s, and expanding into patient advocacy and writing in your 40s. What advice would you give to someone thinking about making a major change?
Change is inevitable and is necessary. You are dying if you are not changing. Embrace the change and imagine the positive outcome before getting in, rather than focusing on the nervousness. Is my thought expanding or contracting? Ask that question constantly and know: contracting thoughts won’t open the doors.
Life is always ‘-ing’ — in progress.
With your older two children in college, what’s been your own experience with the transition? Is it hard to let go?
There is always a challenge in parenting. I think parenting is the most difficult job you can have. My kids both went to schools in drivable distance, so I see them more often than if they were in much farther distances so that helps. However, I know they are God’s sons and He will protect them. I trust that and it will work 100% if they are open.
You wrote an Open Letter to Oprah after reading the book she co-authored with Bruce D. Perry: What Happened to You? How did you know it was the right time for you to open up about your painful early life experiences?
I have been quite open about my life all along to people in general but some are so deep down and traumatic that you are so used to hiding it. I think your intuition tells you when and writing has helped me liberate agonies of hiding and repressing.
In Taking Care of Your Spirit and Realizing the Power of Prayers, you write about the importance of faith. How do you balance faith living in a secular world?
Faith has been saving my life all along. I wouldn’t probably be here if I didn’t have faith. I don’t have balance in a way because I mostly seek God in anything and everything.
I’m curious about your own style. What makes you feel most beautiful and most yourself? Have you changed anything up recently?
Interesting question! As I age, I like brighter colors and I love to coordinate colors as highlights. The world is too colorful to remain dark, although black and white used to be my favorite colors. I think your preference changes with your mindset too. I think in my black-and-white period I used to judge people more than now.
So much of your work deals with really hard topics and traumatic experiences. What kind of activities do you like to do purely for fun? Do you have a binge-watching rec?
I love walking in nature and noticing little things that I used to just pass by. I love painting and I would love to do more. Visiting museums is always fascinating to me. I wish I had time for binge-watching!
So you started writing in your 40s during a difficult time. “Medium was part of my therapies, a space to be creative and express it,” you explained in a post. After nearly three years of writing essays, informative and reported pieces, and poetry, where are you on your healing journey, and how has writing helped?
I love poetry so much that I am writing just poetry these days. I started writing on Medium with the specific goal of writing a book on patient safety with Dr. Heon-Jae Jeong in S. Korea who wrote the book called I am Cheese — the name of my blog for patient safety.
My personal blog ended up becoming a space where I express myself creatively. Poetry is great in creating space for yourself and the reader, no need to be perfect in grammar, and simple. Someone wise said truths in life are very simple and I think poetry does just that. Many poets are activists too, like Maya Angelou, Amanda Gorman, to name a few. Healing can take a long time, perhaps forever, but it is so worth it because you deserve love.
For more, follow Soojin on X (Twitter), LinkedIn, and Medium. Soojin welcomes healthcare stories about empathy and patient safety. You can email your story or questions to jun.soojin@gmail.com for sharing on “I am Cheese.”









I can resonate with this deeply. I learned a lot about the shortcomings of eldercare and the healthcare system when I was going through it with my dad. Because of the language barrier and the cultural gap, It was especially difficult trying to find place for him. That was three years ago and I'm still trying to make sense of it. Eldercare in this country is woefully lacking and so very expensive. I worry a lot about this and the future as we all grow older as a country.